Support Page Content
Concussion Recovery & Resource Project
About the Concussion Recovery & Resource Project
The primary goal of the project is to develop an experiential, interdisciplinary program that supports the missions of Sacramento State as an Anchor University and the College of Health and Human Services Center for Health Practice Policy and Research to impact community health by promoting collaboration, inter-disciplinary practice, and innovation to reduce health inequities in California’s capital region. while fostering student learning and facilitating student engagement within and across Colleges of the University, with the following objectives:
- Disseminate content of concussion-related topics to students so they can describe, discuss, and create educational content which reflects best practice for the medical and rehabilitative management of individuals following concussion
- Improve student engagement within and across Colleges of Sacramento State to address the needs of the public with respect to a major public health issue
- Dispel public misconceptions of concussion-related topics
- Address gaps in knowledge of healthcare providers in the community who provide medical and rehabilitative care for individuals who have sustained a concussion/mTBI
Dispelling Public Misconceptions about Concussion
Despite the high prevalence of concussion, there is a lack of sound, reasonable, and evidence-informed information for concussion-related topics available for public consumption. Individuals who are slow to recover and experience long-term disability following a concussion are often misled by the Internet [Knight et al. Interact J Med Res. 2015], and more specifically on social media and youTube [Williams et al. Br J Sports Med. 2014]. For instance, Kollia et al. found that among 98 of the most widely viewed videos, available through television, social media applications, and internet sites, none were uploaded by a professional source [Kollia et al. Int J Prev Med. 2018].
The lack of sound information for the public has led to misconceptions and misinformation toward concussion-related topics. It has been proposed that such misconceptions may be perpetuated by inefficiencies in concussion education [Merz et al. Archives of Clinical Neuropsychology. 2017], which includes the potential misinformation delivered by healthcare providers to patients. Although the article may be somewhat dated, Stoller et al. revealed that only some, and not all, physicians responsible for the management of individuals following concussion were aware of the existence of a best practice guideline for care for individuals following concussion [Stoller et al. Can Fam Physician. 2014]. Therefore, in addition to unsatisfactory information delivered through media, patients are at risk of receiving inconsistent guidance about concussion from their healthcare providers, further perpetuating misconceptions and confusion as to what may be done to return patients to meaningful activities following a concussion [Damji et al. Concussion. 2018].
Primary sources for misconceptions in Concussion: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6331705/citedby/
What is a Protracted Recovery?
What is Postconcussive Syndrome (PCS) and Persistent Post-concussive Symptoms (PPCS)?
While most adults and children feel better after a concussion within a few days or weeks, 10-33% of people can have symptoms that last for longer than expected. This is frequently called PCS. However, different health associations have different criteria to diagnose PCS. Persistent postconcussive symptoms is a general term that refers to a variety of symptoms frequently experienced following concussion.
- Adults (>18 years old) have PPCS if they continue to have symptoms for greater than 2 weeks after concussion.
- Children (0-18 years old) have PPCS if they continue to have symptoms longer than 4 weeks after concussion.
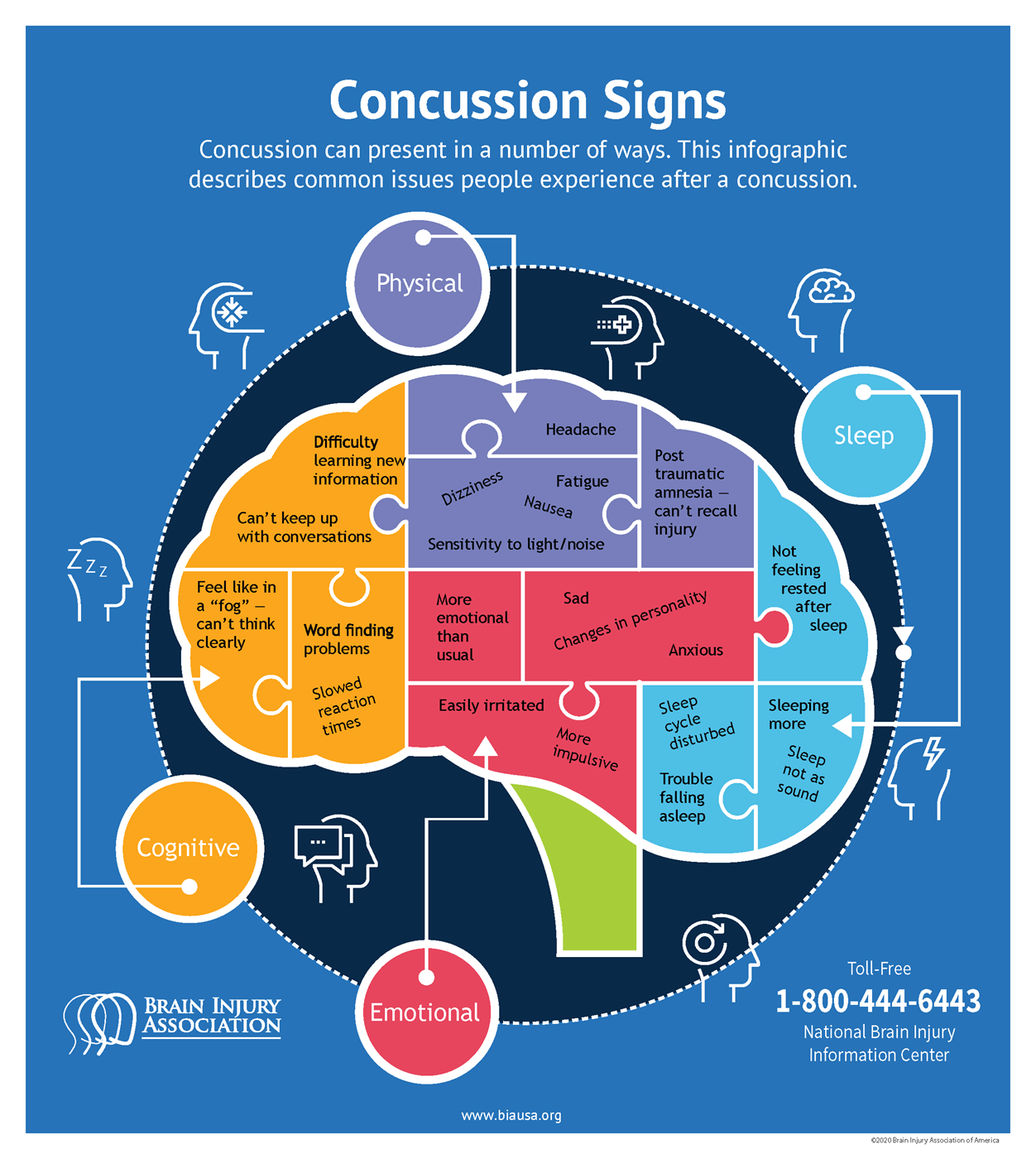
If you sustained a concussion more than two weeks ago and are noticing lingering symptoms of:
- headache
- dizziness
- confusion
- difficulty concentrating
- mental fog
- fatigue
- memory problems
- vision problems
- eye strain
- depression
- anxiety
- social withdrawal
You may be one of 3 million Americans with PPCS. PPCS is characterized by concussive symptoms that last more than 10-14 days in adults and over 4 weeks in children. If you or a loved one are experiencing persistent symptoms, it's time to get re-evaluated by your primary care physician!
For more information about PCS and PPCS:
| Resource | Link |
|---|---|
| Ontario Neurotrauma Foundation: Comprehensive overview of concussion and common prolonged symptoms following concussion, designed specifically for patients: | https://braininjuryguidelines.org/concussion/index.php?id=154 |
| Mayo Clinic concussion information: | https://www.mayoclinic.org/diseases-conditions/post-concussion-syndrome/symptoms-causes/syc-20353352 |
| Concussion Foundation information: | https://concussionfoundation.org/PCS-resources/support |
| Comprehensive Fact Sheet: | https://www.neurosymptoms.org/post-concussion-syndrome/4594358012 |
Is my care reflective of Best Practice?
Annual lifetime cost of TBI is estimated to $945 million, 31% going into medical treatment costs and 69% into lost productivity costs. This heavy financial burden on the healthcare system may be exacerbated by a lack of concussion training, limiting medical and healthcare professionals' abilities to employ best practices for diagnosis and management, thereby leading to unnecessary referrals to specialists and longer recovery time.
Additionally, important deficiencies in the concussion curriculum of Canadian and American medical schools have been identified in several studies. Although the majority of medical students and residents are able to correctly define what a concussion is, they have difficulties correctly identifying concussion symptoms and optimal diagnosis and management strategies, lack the practical experience with concussion diagnosis and treatment, and have never attended a lecture about concussion during their university training.
Similarly, a significant proportion of physicians provide concussion recommendations that are not in line with current evidence-based guidelines. For example, recent changes in concussion treatment best practices include resting with limited cognitive and physical activity for 24 to 48 hours after injury, yet several physicians report not consistently recommending any cognitive or physical rest after a concussion. Source: Babul et al. J Sports Med (Hindawi Publ Corp). 2020
Connecting with Researchers & Educators via Social Media
| YouTube | |||
|---|---|---|---|
| Concussion.Org | Concussion Legacy Foundation | ||
| International Concussion Society | |||
| Concussion Awareness Training Tool | |||
| Katheryn Schneider, Associate Professor, Univ of Calgary | |||
| Christopher Giza, Physician Researcher, Pediatric Sports Concussion Program, UCLA |
Related Literature
Dr. Joyce Mikal-Flynn,
Traumatic Brain Injuries: An Overview
A concussion is a type of traumatic brain injury—or TBI—caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. This sudden movement can cause the brain to bounce around or twist in the skull, creating chemical changes in the brain and sometimes stretching and damaging brain cells. Medical providers may describe a concussion as a “mild” brain injury because concussions are usually not life-threatening. Even so, the effects of a concussion can be serious.
Source: Centers for Disease Control and Prevention (CDC). (2020, September). Traumatic Brain Injury & Concussion: Get the Facts About TBI.
What happens when you have a concussion? (Video)
Concussion sings & symptoms (Video)
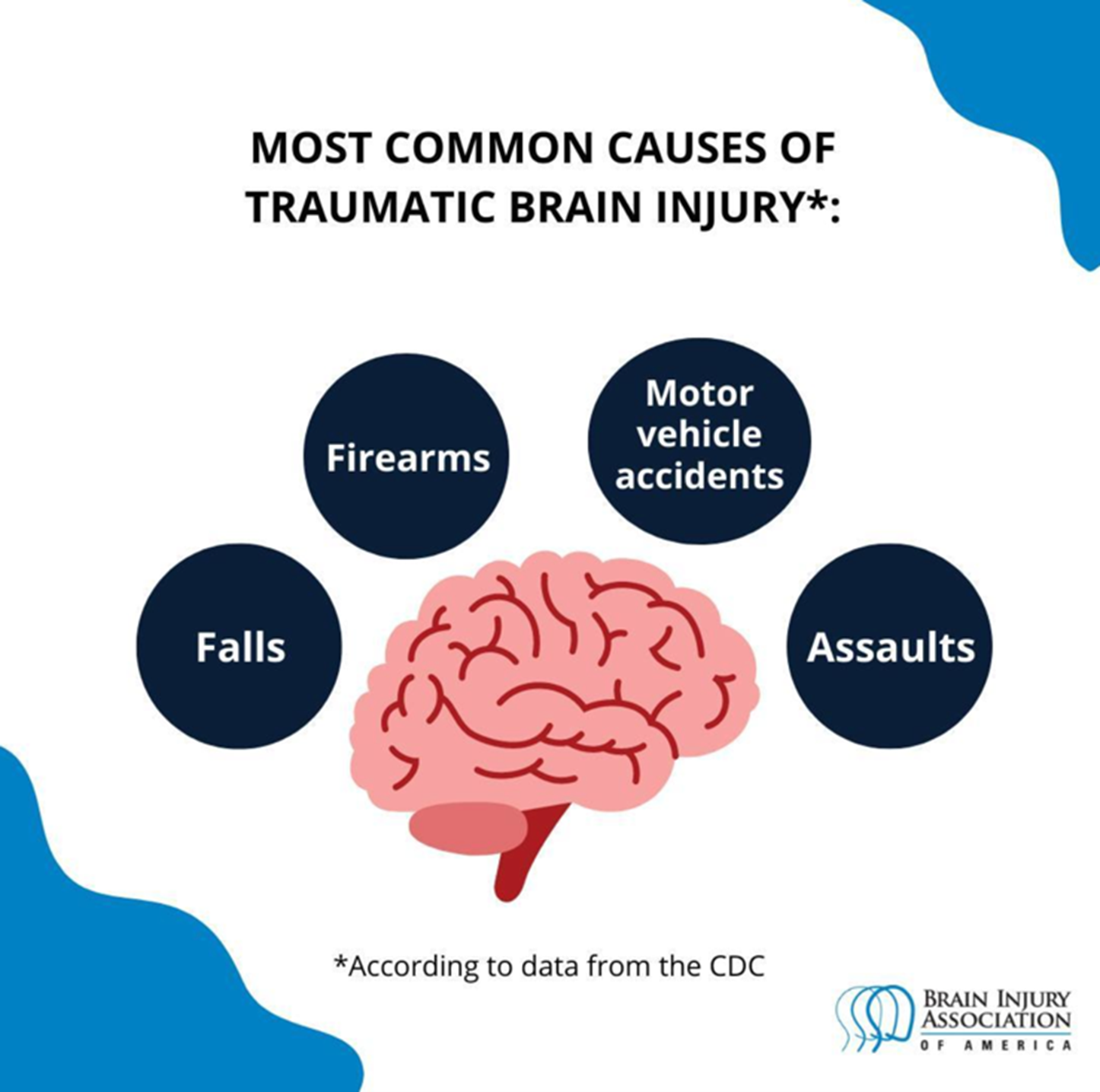
According to the Centers for Disease Control and Prevention (CDC), "A traumatic brain injury, or TBI, is an injury that affects how the brain works that may be caused by a bump, blow or jolt to the head. TBI is a major cause of death and disability in the United States" (CDC, 2020). There are three main types of TBI: mild TBI or concussion (mTBI), moderate TBI, and severe TBI. With over 2 million occurrences and approximately 50,000 deaths annually, TBI is the leading cause of death in young adults (<45 years of age). TBI is associated with $76.5 billion in direct and indirect medical costs (Siebold et al., 2018). Anyone can experience a TBI, but statistics suggest that particular groups are at a higher risk of obtaining a TBI or having poorer health outcomes after the injury. The CDC states that groups who are more likely to be affected by TBI include: racial and ethnic minorities, service members and veterans, people who experience homelessness, people who are in correctional and detention facilities, survivors of intimate partner violence, and people living in rural areas (CDC, 2020).
Individuals may acquire a TBI from various accidents; however, the most common TBI injuries result from falls, firearm-related injuries, motor vehicle crashes, and assaults (CDC, 2020). The effects of these injuries can lead to short-term or life-long health and cognitive-communication challenges. For example, initial and persistent cognitive-communication deficits are the most common complaints after TBI and the biggest challenge to independent living, social re-adaptation, engagement in family life, and participation in everyday activities (McAllister et al., 2004). Individuals may frequently demonstrate cognitive deficits such as diminished memory for spatial information, decreased divided attention skills, working memory deficits, and impairments in general attention, problem-solving, and memory skills (Childers & Hux, 2016). Prevalence estimates of memory impairment in TBI range between 54 and 84%. Memory impairment can negatively impact and reduce the quality of life, and memory impairment varies across individuals with similar injury severity. Recent evidence suggests that working memory capacity may be one mediating variable that can help explain why cognitive reserve protects against long-term memory impairment (Sandry et al., 2014).
Types of Traumatic Brain Injuries
The Department of Defense (DOD) defines the following levels of severity (Defense Health Agency, 2019):
- Concussion/Mild TBI—loss of consciousness for up to 30 minutes; or confused or disoriented state lasting less than 24 hours; or memory loss lasting less than 24 hours. Excludes penetrating TBI. Results of a computed tomography (CT) scan, if obtained, are normal.
- Moderate TBI—loss of consciousness for more than 30 minutes, but less than 24 hours; or confused or disoriented state lasting more than 24 hours; or memory loss lasting more than 24 hours but less than 7 days; or meets criteria for concussion/mild TBI but with an abnormal CT. Excludes penetrating TBI. A structural brain imaging study may be normal or abnormal.
- Severe TBI—loss of consciousness for more than 24 hours; or confused or disoriented state lasting more than 24 hours; or memory loss lasting more than 7 days. Excludes penetrating TBI. A structural brain imaging study may be normal but usually is abnormal.
- Penetrating TBI—open head injury; scalp, skull, and dura mater (outer layer of meninges) are penetrated. Caused by high-velocity projectiles, objects of lower velocity such as knives, or bone fragments from a skull fracture that are driven into the brain.
Podcast Series
This podcast series’ primary focus is to spread awareness about TBI. Throughout these episodes, individuals will share their own experiences and stories. Professionals, caregivers, and TBI survivors share their insights and bring to light living with and caring for a TBI.
I Have a TBI

TBI Survivor - Tatiana
Tatiana is a practicing artist and aspiring mathematics teacher. She resides in Davis, California and attends California State University, Sacramento. She suffered a TBI in 2017 after an automobile accident.
General Resources
- Quick Guide to Traumatic Brain Injury
- Mild Traumatic Brain Injury and Concussion: Information for Adults
- University Hospitals: Basic Information About Traumatic Brain Injury

TBI Survivor - Eric Williams
Eric is a full-time fire prevention officer. He is a father and resides in Folsom, California. He suffered a TBI in 2015 after a running and bicycle accident.
Support Group Resources
- A Guide to Northern California Resources for Individuals with Brain Injury
- Del Oro Resource Center: Support Groups - Sacramento County
- Toolkit for TBI Support Group Facilitators

Mother of a TBI Survivor - Donna Long
Donna is a mother of three children and resides in the Sacramento area. She has been the primary caretaker of her son who suffered a TBI in 2019. She has been an advocate for her son and is motivated to share her experience to increase TBI awareness.
Caregiver & Family Resources
- BIUSA: Challenges, Changes, and Choices: A Brain Injury Guide for Families and Caregivers
- Mayo Clinic: Understanding Brain Injury - A Guide for the Family
- BIAUSA: Adults & Brain Injury - Financial Issues
- Navigating the Insurance Maze after Brain Injury: a guide for patients and their advocates
- BIAUSA: Is financial assistance available to people with brain injury and their families?

Physiatrist - Dr. Topher Stephenson M.D.
Dr. Topher Stephenson, M.D. graduated from the University of New Mexico School of Medicine completed his residency in Physical Medicine & Rehabilitation at the University of California, Davis. Dr. Stephenson is board certified in both Physical Medicine & Rehabilitation and Brain Injury Medicine.

Speech-Language Pathologist - Elisabeth (Lisa) D'Angelo, M.S. CCC-SLP CBIS
Bio Coming Soon

Speech-Language Pathologist - Shannon Gassuan, M.S. CCC-SLP CBIS Veteran Affairs
Bio Coming Soon
Veteran's Resources
- Resources for Caregivers of Veterans with Traumatic Brain Injury
- Military Health System: A Guide for Caregivers of Service Members and Veterans
- I’m Caring for a Veteran with a Traumatic Brain Injury (TBI)- What do I need to know?

Speech Language Pathologist - Denise Kendrix, M.A. CCC-SLP
Denise graduated from the University of Redlands with a Bachelor of Arts degree in Communication Disorders and earned her Master of Arts degree in Speech Language Pathology from San Jose State University. She has worked in the medical setting for over 20 years with adults with cognitive, communication and swallowing disorders. She has a primary focus in traumatic brain injury and stroke and assists with facilitating the UC Davis Traumatic Brain Injury Support Group. She also is a volunteer board member for the Medical Speech Council of California.

Physical Therapist - Katie Shinoda, DPT
Dr. Shinoda is a physical therapist at Mercy Outpatient Rehabilitation Center in Citrus Heights, California. She has been a practicing physical therapist for over 20 years and works with TBI and other neurologic disorders. She has worked in various stages of rehabilitation and recovery, including acute care, intensive care unit, and outpatient services. She currently practices physical therapy with individuals diagnosed with TBI and vertigo. She also organizes a grant-funded program for additional services for people with TBI trying to reintegrate into society.

Registered Nurse - Alyssa Francis
Alyssa is a registered nurse at UC Davis Medical Center in Sacramento, California. She works in the medical surgery unit trauma patients including TBI. She is passionate about caring for and education patients and their families.
- Mild Traumatic Brain Injury Rehabilitation Toolkit
- Traumatic Brain Injury: A Guidebook for Educators
- Barrow Neurological Institute & Dignity Health: Traumatic Brain Injury Patient and Family Handbook
Books & Literature
The following books are recommended for those looking to learn more about traumatic brain injuries:
- "You Look Great!" - Strategies for Living Inside a Brain Injury
- Turn the Lights On!: A Physician’s Personal Journey from the Darkness of Traumatic Brain Injury (TBI) to Hope, Healing, and Recovery
- Our Daddy Is Invincible!
- Stroke Recovery Activity Book - Puzzles Workbook for Traumatic Brain Injury & Aphasia Rehabilitation
- Understanding Traumatic Brain Injury: A Guide for Survivors and Families
- Honey, I Smell Flowers